Stage IV Pressure Injury
Initial
Assessment

Content may be considered graphic.
Click to ViewWeek 1 9.5 cm x 6.7 cm x 3 cm

Content may be considered graphic.
Click to ViewWeek 3, 7.3cm x 4cm x 1.9cm

Content may be considered graphic.
Click to ViewWeek 4 5.9 cm x 3.8 cm x 1 cm

Content may be considered graphic.
Click to ViewWeek 5 2.5 cm x 1.8 cm x .6 cm

Content may be considered graphic.
Click to ViewBackground
Operating Room acquired pressure injury prevalence is well documented over 8% of total surgeries for procedures over 3 hours. The total cost to treat such injuries can range from $14,000 to $40,000 per patient and is not reimbursed by Medicare. Repositioning the patient during long surgeries often proves challenging, which may result in a pressure injury from prolonged pressure over bony prominences.
A 43-year-old female acquired a stage IV pressure injury over her right scapula after a 21-hour surgery. The patient had contracted necrotizing fasciitis which required extensive surgery to attempt to save her life and limbs.
The pressure injury presented the day following surgery. The wound measured 10.2 cm x 7.6 cm x 3.8 cm (length x width x depth). The wound bed was clean. Initial treatment was to pack the wound with a hydrogel gauze with a cover dressing, changed every four days.
Intervention
Gladiator Therapeutics infrared therapy was initiated to accelerate the healing of the stage IV pressure injury. Infrared therapy assists to reduce inflammation and increase microcirculation to provide the wound with greater blood flow and nutrients for faster healing. The patented infrared ceramics were utilized approximately 6 hours per day for maximum exposure.
Results
When the initial wound assessment was conducted by hospital staff, it was estimated that it would take approximately 3 months to heal a wound of this size with standard dressings.
Significant signs of improvement were noted by week two of initiating the protocol. By week three, the wound had significant granulation tissue, and the wound was approximately 50% smaller in length, width, and depth. The healing continued to progress and the wound was completely healed within 6 weeks.
Reference: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4467017/
Failing Muscle Flap
Initial
Assessment

Content may be considered graphic.
Click to View2 Weeks

Content may be considered graphic.
Click to View3 Weeks

Content may be considered graphic.
Click to ViewBackground
Patient is a 58-year-old female with diabetes. The patient had muscle flap surgery to repair a surgical site on the left thigh due to the excision of a cancerous tumor. The surgeon used adjacent skin and tissue near the wound, to cover the wound. The flap was attached to the original site with its retained blood supply. With diabetes patients, there is a greater risk of failure as the narrowed blood vessels lead to decreased blood flow and oxygen to the surgical site.
Additionally, elevated blood sugar level decreases the function of red blood cells that carry nutrients to the tissue. This lowers the ability of the white blood cells to fight infection. Without sufficient nutrients and oxygen, the surgical site heals slowly and is at greater risk of infection.
Upon the initial assessment for the case the surgical site was becoming necrotic with black eschar tissue, indicating a lack of blood flow to the site. Erythema was observed around the wound indicating possible signs of infection. The patient had planned to have a subsequent skin graft surgery when Gladiator infrared therapy was recommended as an alternate treatment option.
Intervention
Gladiator Therapeutics infrared therapy was initiated to accelerate the healing of the failing flap surgery. Infrared therapy assists to reduce inflammation and increase microcirculation to provide the wound with greater blood flow and nutrients for faster healing. The patented infrared ceramics were wrapped around the leg and utilized approximately 5 hours per day.
Results
Evidence of increased circulation was visible within the first few days of utilizing the Gladiator device. The eschar tissue quickly sloughed off, revealing granulation tissue underneath. The surgical site continued to progress until it was healed at three weeks. Utilization of the Gladiator device helped this patient avoid the cost and pain associated with a second surgery.
Diabetic Foot Ulcer/Blister
Initial
Assessment

Content may be considered graphic.
Click to ViewDay 2

Content may be considered graphic.
Click to ViewDay 4

Content may be considered graphic.
Click to ViewBackgournd
Patient is a 31-year-old female with Type II diabetes and a history of foot wounds over the past 12 months. The patient has compromised blood flow and neuropathy as a result of her diabetes. Shortly after the diabetes diagnosis, a foot ulcer developed on the bottom of her right foot caused by prolonged pressure from standing. An off-loading boot was prescribed and the wound took over 6 months to heal. A blister on the left foot developed shortly after, as a result of friction. The blister measured 3.2 cm x 5 cm x .1 cm (length x width x depth). The blister was drained and the skin was removed. There were no signs of infection and a gauze dressing was applied and changed 2 times a day.
Intervention
Gladiator Therapeutics infrared therapy was initiated. Infrared therapy assists to reduce inflammation and increase microcirculation to provide the wound with greater blood flow and nutrients for faster healing. The patented infrared ceramics were utilized approximately 12 hours per day. The device was placed on the foot upon her return home from work and was removed the following morning.
Results
The prevalence of foot ulcers for persons with diabetes is estimated at 25%. Efficient treatment of diabetic foot ulceration is essential in order to avoid limb amputation and preserve the quality of life. There is a strong correlation between diabetic foot ulcers and leg amputations, as diabetes is the cause of almost 50% of all nontraumatic lower-extremity amputations worldwide.
Two days after employing the Gladiator device, there was evidence of reduced inflammation and less fluid in the blister. On day four, the top layer of skin was removed and revealed healthy granulation tissue underneath. The patient was relieved and hopeful that she now has a treatment option that can help manage her wounds, and avoid a possible amputation in the future.
Reference: https://www.woundsresearch.com/article/8706
Venous Stasis Ulcer
16-08-2019
Medial

Content may be considered graphic.
Click to View23-12-2019
Lateral

Content may be considered graphic.
Click to View20-01-2020
Medial

Content may be considered graphic.
Click to View20-01-2020
Lateral

Content may be considered graphic.
Click to ViewBackgournd
Patient is a 60-year-old male with Type II diabetes and a history of chronic bilateral venous stasis ulcers on the lower right leg. The current episode has resulted in no improvement in healing in the past 12 months. The patient is being treated by a vascular surgeon at a hospital-affiliated wound clinic. The wound is being treated with an antimicrobial calcium alginate dressing and a compression wrap. In addition to diabetes, the patient was immobile and has a renal deficiency, and surgical interventions have been postponed as a result.
Intervention
Gladiator Therapeutics infrared therapy was initiated to stimulate wound healing. The device was worn over the compression wrap with the limb elevated for 2-4 hours per day. After two weeks, the patient developed more sensation over the wound so the device was moved just adjacent to the wound. Additionally, a second device (Gladiator Mini) was utilized on the patient’s leg to increase circulation in the entire limb. At four weeks, a third device (Gladiator full-size blanket) was added and worn on the abdomen to treat the patient systemically with far infrared.
Discussion & Results
Venous stasis ulcers can take months to heal, and in some cases, they never heal. Treatment generally focuses on improving circulation to the tissue through compression, or in some cases surgical intervention. In this case, surgery was not a viable option due to the patient’s overall condition. Compression had been utilized for a year with no success. At the start of the trial, the wound measured 6.5 cm x 9.2 cm x .3 cm (length x width x depth). There was significant slough and eschar tissue covering the wound bed. The Gladiator devices were employed on Sept 10, 2021 and significant changes occurred in the wound within two weeks. Slough and eschar tissue continued to diminish as fresh granulation and epithelial tissue developed. The wound continued to progress and at four months was reduced to measuring 4.5 cm x 2.3 cm x .2 cm (length x width x depth).
Other health benefits were also realized by the patient. Over this period the patient had more energy, improved his mobility, and kidney function normalized. There were no other medical interventions implemented during this time to account for the improvements other than the benefits of the Gladiator therapy.
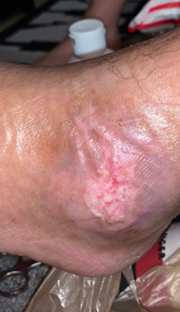
Diabetic Foot Ulcer/Chronic
Initial
Assessment

Content may be considered graphic.
Click to ViewInitial Assessment
2/2/20

Content may be considered graphic.
Click to View2/9/20

Content may be considered graphic.
Click to View2/20/20

Content may be considered graphic.
Click to ViewBackgournd
Patient is a 38-year-old male with type 2 diabetes since 2010. Additionally, the patient has confirmed coronary artery disease as of 2019 and peripheral artery disease diagnosed in 2020. The patient’s wound was due to a suspected fracture of the 5th metatarsal on the right foot.
In December 2019, a dime-sized eschar was noted on the lateral right foot. This wound remained stable for approximately two weeks until the wound rapidly grew in size. There was also increased pain and swelling at that time. The patient went to the emergency department and an arteriogram confirmed peripheral artery disease. There was no pulse in the foot. Toes were dark purple on top indicating a lack of circulation. Patient underwent multiple debridements at the end of January 2020.
Intervention
Gladiator Therapeutics infrared therapy was initiated on February 2, 2020. The wound had undermining at the 5 o’clock position. A calcium alginate dressing with foam cover dressing was used to dress the wound. The peripheral edges of the wound had some remaining eschar tissue.
Results
Overall circulation improved significantly. Over the 18-day-period, the wound continued to develop granulation tissue and there was now a pedal pulse and good perfusion noted after consistent use of the Gladiator device. Circulation extended to the toes which were also showing improvement.
Diabetic Foot Ulcer/Hammertoe
02-08-2020
Bottom of toe

Content may be considered graphic.
Click to View03-07-2020
Bottom of toe

Content may be considered graphic.
Click to View02-08-2020
Top of toe

Content may be considered graphic.
Click to View03-07-2020
Top of toe
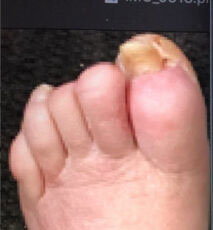
Content may be considered graphic.
Click to ViewBackgournd
Patient is a 58-year-old female with a history of type 2 diabetes, osteomyelitis, neuropathy, hammertoes, thyroid issues, afib, and high blood pressure which is being treated medicinally.
For this patient, hammertoes increase the risk of ulcers. When patients have significant neuropathy, the muscles no longer receive instructions from the nerves, so they start to shrink and weaken. With diabetic neuropathy, the foot muscles weaken first, and without foot muscles to stabilize the toes and keep them somewhat straight, the toes end up becoming contracted over time. This can lead to calluses and ulcers from pressure and friction of the deformed toes.
The patient presented with a left foot ulcer on the big toe in Feb/March of 2019, caused primarily due to pressure from hammertoes. There was no healing progress for almost a full year. The wound was dry with evidence of eschar from the three o’clock to six o’clock position. The overall condition of the foot and the color of the skin shows compromised circulation.
Approximately 6 years prior, 2 toes were partially amputated on the same foot due to this condition.
The initial treatment used was antibiotics and calcium alginate to dress the wound. The patient battled sepsis all summer. In October 2109, an aggressive antibiotic treatment (6 antibiotics) was prescribed. This treatment helped with the infection but did nothing for the hammertoe ulcer. She also took Cymbalta for neuropathy.
Intervention
On December 6, 2019, the patient began using Gladiator Therapeutics technology in an attempt to heal the wound on the big toe and address neuropathy. The patented infrared ceramics were wrapped around the distal end of the foot. She wore the therapy approximately 23 hours per day, only removing it to shower/bath. No other therapies were utilized.
Results
Infrared therapy successfully reduced inflammation and increased microcirculation to provide the wound with greater blood flow and nutrients. One month after initiation of the Gladiator therapy, the wound has filled in with new tissue and there is no evidence of eschar remaining. The toes are also less swollen and the color change of the skin is evidence of improved circulation overall in the foot. Additionally, there were no more phantom pains from neuropathy.
Raynaud’s & Scleroderma
3/13/20

Content may be considered graphic.
Click to View3/18/20

Content may be considered graphic.
Click to View3/23/20

Content may be considered graphic.
Click to View4/6/20

Content may be considered graphic.
Click to View4/8/20

Content may be considered graphic.
Click to View4/11/20

Content may be considered graphic.
Click to View5/18/20
Content may be considered graphic.
Click to View6/1/20

Content may be considered graphic.
Click to ViewBackgournd
Patient is a 24 year old African American female with a diagnosis of both Raynaud’s and Scleroderma in both hands and feet.
Patients with Raynaud’s disease experience numbness and coldness in fingers, feet, and toes in response to cold temperatures or stress. During an attach, smaller arteries that supply blood to the skin narrow, limiting blood circulation to affected areas. This secondary diagnosis of Sclerodema further complicates wound healing as it results in the hardening of the skin.
The wound presented in early November 2019. It has continuously gotten worse and has not responded to any treatment prior to starting the Gladiator Therapeutics therapy.
Intervention
Gladiator Therapeutics infrared therapy was initiated to kick start healing on 3/13/2020. A mini blanket was used on her left thigh and a five ceramic device on the wound. The patient wore the devices for 10 to 12 hours a day.
Results
Within only 5 days the patient experienced increased sensitivity in both legs as a result of increased blood supply to the foot. In 10 weeks the wound was completely healed.
Melanoma Skin Cancer
Day of
surgery

Content may be considered graphic.
Click to ViewDay after
surgery

Content may be considered graphic.
Click to View3 weeks after
surgery

Content may be considered graphic.
Click to View6 weeks after
surgery

Content may be considered graphic.
Click to View